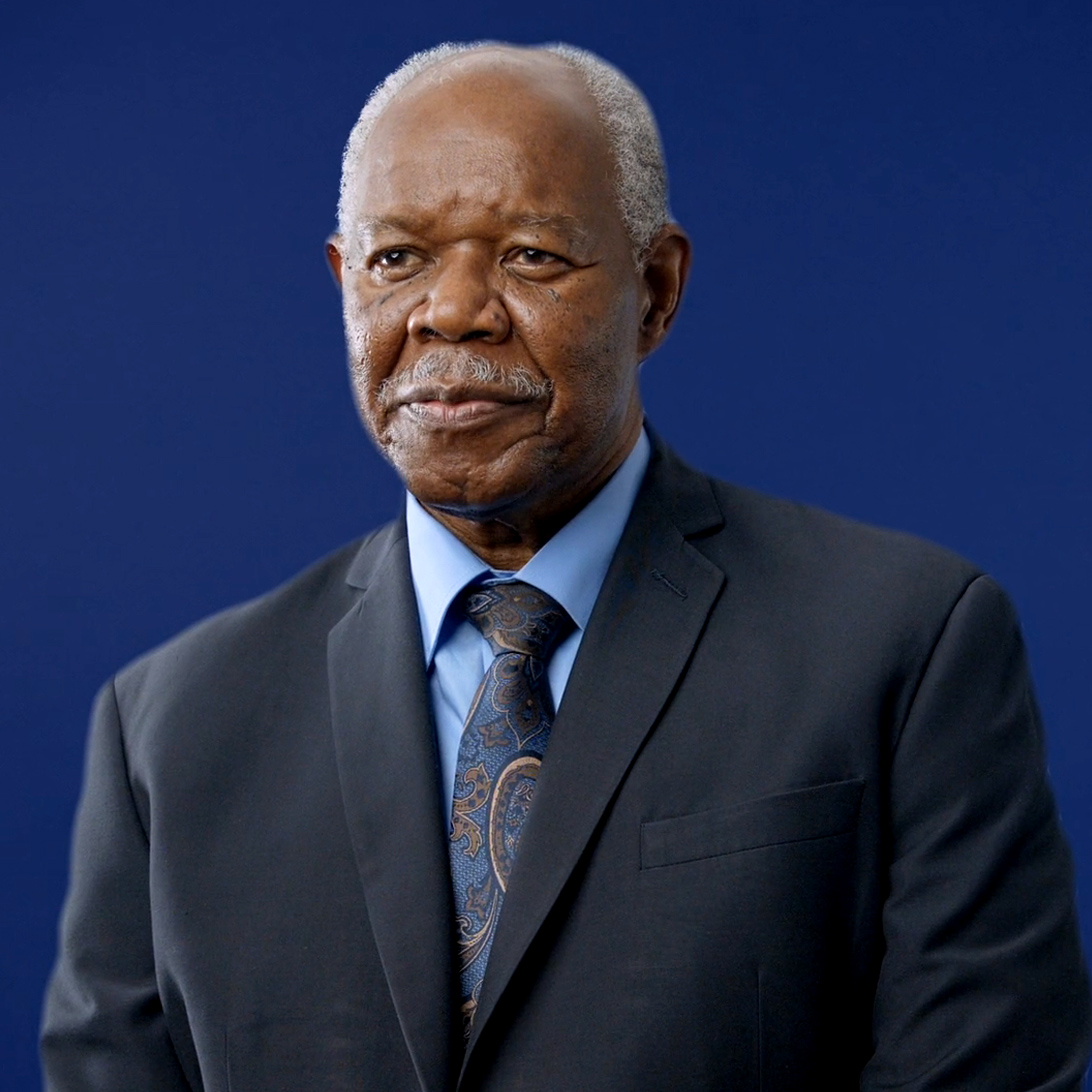
Walter
Prostate Cancer
Walter’s Journey: Challenging Medical Norms in the Face of a Cancer Diagnosis
Walter admits folks from his generation rarely question advice from a doctor.
“When you went to the doctor, you listened to what he or she had to say, did exactly what he or she said, and that was that,” Walter, 77, said.
The vast amount of information available online has turned that way of thinking upside down, shifting the doctor–patient relationship into more of a partnership. It’s a dynamic that Walter credits with extending his life in the face of Stage 4 prostate cancer.
Not every doctor has embraced this trend, and for good reason. The Internet is littered with inaccurate information. But Walter’s story can serve as a case study for how to navigate this new frontier of patient empowerment and self-advocacy.
Walter had some built-in advantages. After a career in finance—including prominent corporate roles at Neiman Marcus, Bloomingdale’s, and Sunglass Hut—Walter chose to become an Emergency Medical Technician (EMT) for the Somers Volunteer Fire Department in New York.
His 17-year background as an EMT made him comfortable reading medical journals and seeking research-based, peer-reviewed information.
Until five years ago, his interest in medical journals served only as a hobby of sorts. That was before Walter’s PSA test jumped from a 4 to a 20. He was told it was an infection and given antibiotics.
Many doctors use a PSA cutoff point of 4 ng/mL or higher when deciding if a man needs further testing to detect prostate cancer. However, Walter’s doctor dismissed his initial rise as an infection and did not feel a follow-up was needed. Walter was told that the National Comprehensive Cancer Network (NCCH) recommended no need to check PSA after the age of 60.
The doctor skipped the next annual PSA, following NCCH guidelines. Unfortunately, Walter followed this advice.
At his next physical, Walter specifically requested a PSA test. It had jumped to an astounding 128, which led to further tests and a Stage 4 prostate cancer diagnosis.
The news came as a shock.
Walter was referred to an oncologist who told him it was too late — while they could attempt hormone therapy, a lymph node containing cancer could not be treated because of the risk of photons damaging normal tissue and organs — mainly the rectum, bladder and bowel. If the lymph node could not be treated, what was the purpose?
“Upon hearing that, I recalled one of Dante’s quotes, ‘Abandon all hope, ye, who enter here,’ ” Walter said. “That is when I became my own healthcare advocate. There had to be some alternatives. I did not want to become incontinent for the rest of my life.”
That is also when his hobby of reading medical journals proved most beneficial.
Walter delved into the realm of online medical resources, leveraging databases like PubMed. Amidst this research, he stumbled upon proton therapy, a treatment option often overlooked and even less understood by conventional medicine.
He learned that proton therapy can reduce radiation exposure to sensitive areas of the body by up to 50% compared to standard X-ray (photon) radiation treatments.
Standard X-ray radiation, or beams of photons, releases its maximum dose and continues to release it as it passes and exits through the body beyond the tumor. By contrast, proton therapy releases its maximum dose directly within the tumor and then stops.
“This fundamental difference makes proton therapy preferential for certain tumors,” Walter said. “If vital organs or structures are along the path the photon radiation travels, heathy tissue will be damaged. Protons cause less damage to the normal cells and tissue, because proton particles release all their energy at the tumor. There is no exit radiation to cause damage to the nearby healthy tissues. That made sense to me, and I thought it might solve my lymph node issue.”
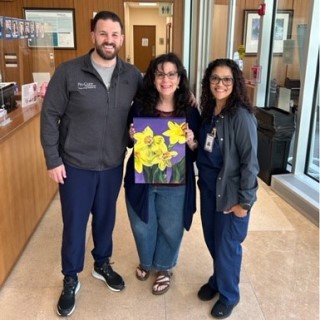
Armed with this newfound understanding, Walter sought treatment at ProCure Proton Therapy Center in Central New Jersey. Walter immediately noticed the positive, upbeat manner in which the ProCure staff welcomed him.
Dr. Jae Y. Lee was Walter’s oncologist and made him feel like a valued individual.
“Feeling valued is the common thread that binds us all,” Walter said. “Respect leads to value. Value leads to trust. At ProCure, it was like I walked into a different world.”
ProCure doctors used pencil beam scanning to directly target his lymph node. Walter said he experienced only minor side effects during the eight weeks of treatment. His typical appointment, including treatment time, took about 45 minutes.
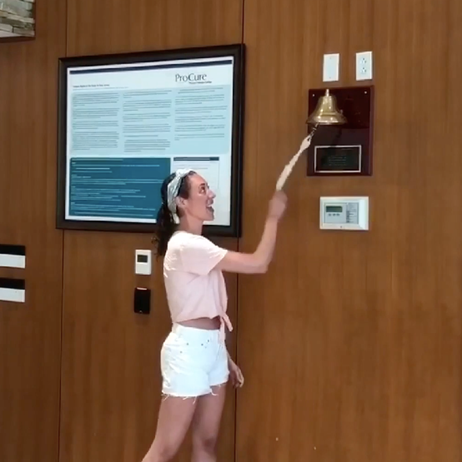
After his treatment, Walter visited his urologist for another PSA test. The urologist seemed puzzled by the results.
“There’s something wrong with this,” Walter remembers the urologist telling him. “These numbers just can’t be right. They’re too low.”
Walter asked his oncologist what he expected the PSA score to be. Walter was told 1.0 or 2.0.
The actual score was 0.033. It was the good news that Walter wanted to hear.
Watler said the treatment he received at ProCure played a role in extending his life. But he said it’s not the only reason. His research led him to change his diet as well, with the goal of keeping his cancer at bay.
So far so good.
“I am not cured because it is Stage 4,” Walter said. “I accept that fact. But people are amazed I’m still walking. I feel healthy and have reached a major milestone of five years after diagnosis.”
Walter continues to explore medical journals and has used what he reads to start a dialog with his doctors.
“Those case studies have actually changed the way several of my doctors have treated me,” he said. “I’m not claiming that I solved it, but we are able to have open discussions as to what was good or bad and I can participate in decisions. They know that I am a self-advocate of my own healthcare, and we now work as a team. In the past, that would not have happened.”